IMPORTANT SAFETY INFORMATION
WARNING: RISK OF THYROID C-CELL TUMORS
In male and female rats, dulaglutide causes a dose-related and treatment-duration-dependent increase in the incidence of thyroid C-cell tumors (adenomas and carcinomas) after lifetime exposure. It is unknown whether Trulicity causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans as human relevance of dulaglutide-induced rodent thyroid C-cell tumors has not been determined.
Trulicity is contraindicated in patients with a personal or family history of MTC and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk of MTC with use of Trulicity and inform them of symptoms of thyroid tumors (eg, mass in the neck, dysphagia, dyspnea, persistent hoarseness). Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with Trulicity.
WARNING: RISK OF THYROID C-CELL TUMORS
In male and female rats, dulaglutide causes a dose-related and treatment-duration-dependent increase in the incidence of thyroid C-cell tumors (adenomas and carcinomas) after lifetime exposure. It is unknown whether Trulicity causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans as human relevance of dulaglutide-induced rodent thyroid C-cell tumors has not been determined.
Trulicity is contraindicated in patients with a personal or family history of MTC and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk of MTC with use of Trulicity and inform them of symptoms of thyroid tumors (eg, mass in the neck, dysphagia, dyspnea, persistent hoarseness). Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with Trulicity.
Trulicity is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2, and in patients with a serious hypersensitivity reaction to dulaglutide or any of the product components.
Risk of Thyroid C-cell Tumors: One case of MTC was reported in a patient treated with Trulicity in a clinical trial. This patient had pretreatment calcitonin levels approximately 8 times the upper limit of normal (ULN). An additional case of C-cell hyperplasia with elevated calcitonin levels following treatment was reported in the cardiovascular outcomes trial (REWIND). If serum calcitonin is measured and found to be elevated or thyroid nodules are noted on physical examination or neck imaging, the patient should be further evaluated.
Pancreatitis: Has been reported in clinical trials. Observe patients for signs and symptoms including persistent severe abdominal pain sometimes radiating to the back, which may or may not be accompanied by vomiting. If pancreatitis is suspected, discontinue Trulicity promptly and initiate appropriate management. Do not restart if pancreatitis is confirmed. Consider other antidiabetic therapies in patients with a history of pancreatitis.
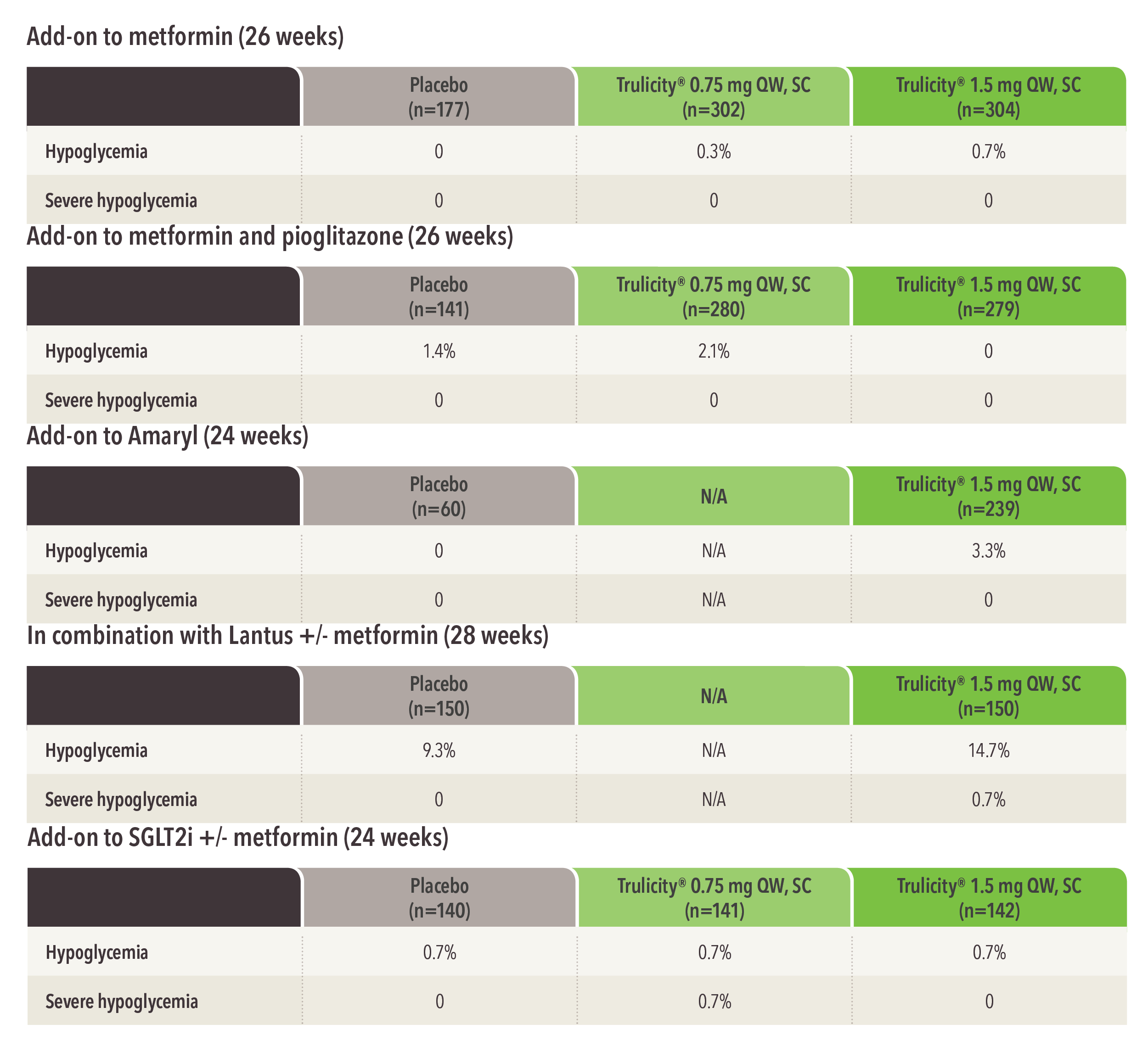
Hypoglycemia: Patients receiving Trulicity in combination with an insulin secretagogue (e.g., sulfonylurea) or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia. The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogue) or insulin. Inform patients using these concomitant medications of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.
Hypersensitivity Reactions: There have been postmarketing reports of serious hypersensitivity reactions (eg, anaphylactic reactions and angioedema) in patients treated with Trulicity. Instruct patients who experience symptoms to discontinue Trulicity and promptly seek medical advice. Trulicity is contraindicated in patients with a previous serious hypersensitivity reaction to dulaglutide or to any of the components of Trulicity. Use caution in a patient with a history of angioedema or anaphylaxis with another GLP-1 receptor agonist as it is unknown whether they will be predisposed to anaphylaxis with Trulicity.
Acute Kidney Injury: In patients treated with GLP-1 RAs, there have been postmarketing reports of acute renal failure and worsening of chronic renal failure, sometimes requiring hemodialysis. A majority of reported events occurred in patients who had experienced nausea, vomiting, diarrhea, or dehydration. In patients with renal impairment, use caution when initiating or escalating doses of Trulicity and monitor renal function in patients experiencing severe adverse gastrointestinal reactions.
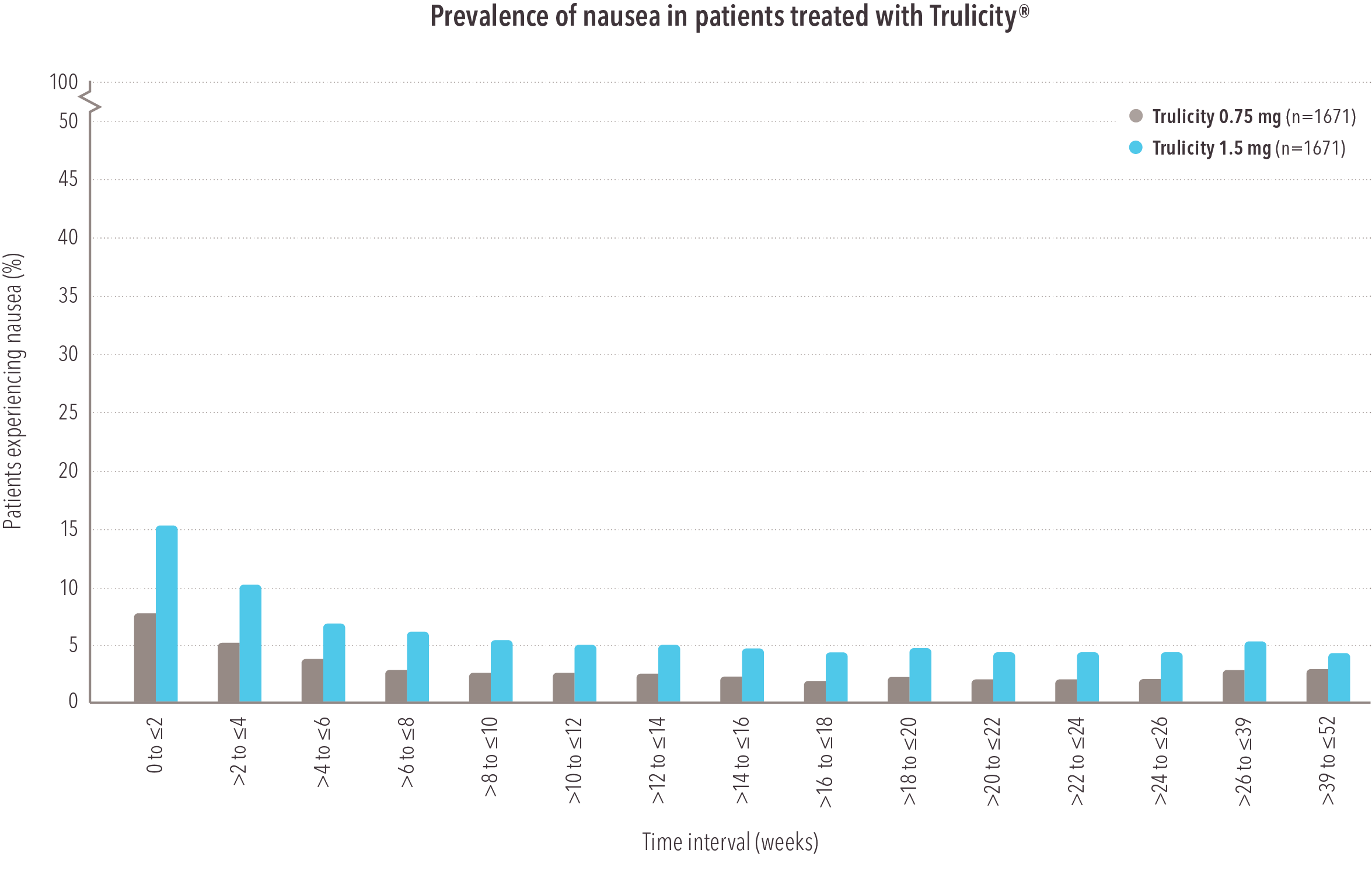
Severe Gastrointestinal Disease: Use of Trulicity may be associated with gastrointestinal adverse reactions, sometimes severe. Trulicity has not been studied in patients with severe gastrointestinal disease, including severe gastroparesis, and is therefore not recommended in these patients.
Diabetic Retinopathy Complications: Have been reported in a cardiovascular outcomes trial. Monitor patients with a history of diabetic retinopathy.
Acute Gallbladder Disease: Acute events of gallbladder disease such as cholelithiasis or cholecystitis have been reported in GLP-1 receptor agonist trials and postmarketing. In a cardiovascular outcomes trial with a median follow up of 5.4 years, cholelithiasis occurred at a rate of 0.62/100 patient-years in Trulicity-treated patients and 0.56/100 patient-years in placebo-treated patients after adjusting for prior cholecystectomy. Serious events of acute cholecystitis were reported in 0.5% and 0.3% of patients on Trulicity and placebo respectively. If cholelithiasis is suspected, gallbladder studies and appropriate clinical follow-up are indicated.
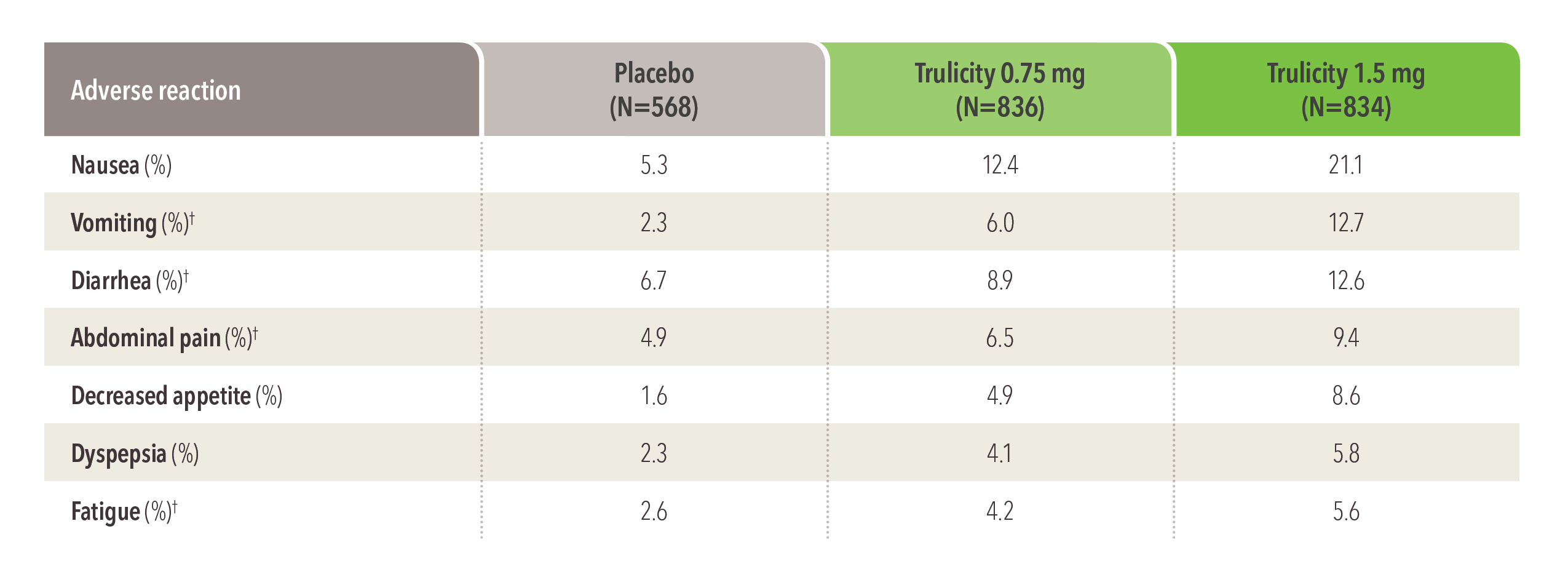
The most common adverse reactions: Incidence reported in ≥5% of Trulicity-treated patients in trials were nausea, diarrhea, vomiting, abdominal pain, decreased appetite, dyspepsia, and fatigue.
Oral Medications and Delayed Gastric emptying: Trulicity slows gastric emptying, which may impact absorption of concomitantly administered oral medications. Use caution when oral medications are used with Trulicity. Drug levels of oral medications with a narrow therapeutic index should be adequately monitored when concomitantly administered with Trulicity. In clinical pharmacology studies, Trulicity did not affect the absorption of the tested, orally administered medications to a clinically relevant degree.
Pregnancy: Limited data with Trulicity in pregnant women are not sufficient to determine a drug-associated risk for major birth defects and miscarriage. Based on animal reproduction studies, there may be risks to the fetus from exposure to dulaglutide. Use only if potential benefit justifies the potential risk to the fetus.
Lactation: There are no data on the presence of dulaglutide in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Trulicity and any potential adverse effects on the breastfed infant from Trulicity or from the underlying maternal condition.
Pediatric Use: Trulicity-treated pediatric patients reported a higher incidence of injection site-related reactions compared to Trulicity-treated adults. Safety and effectiveness of Trulicity have not been established in patients less than 10 years of age.
Please click to access Prescribing Information, including Boxed Warning about possible thyroid tumors including thyroid cancer, and Medication Guide.
Please see Instructions for Use included with the pen.
DG HCP ISI 17NOV2022